Speakers Conference Sponsor
- Prof Lars Bode
- Dr Chris Mullally
- Tracey Sedgwick
- Heidi Thomson RN IBCLC
- Dr Josa Sadler MBBS
- Dr Stuart Prosser MBBS MMed MBA
- Tanya van Aswegen APD, MPH
Bio’s Below



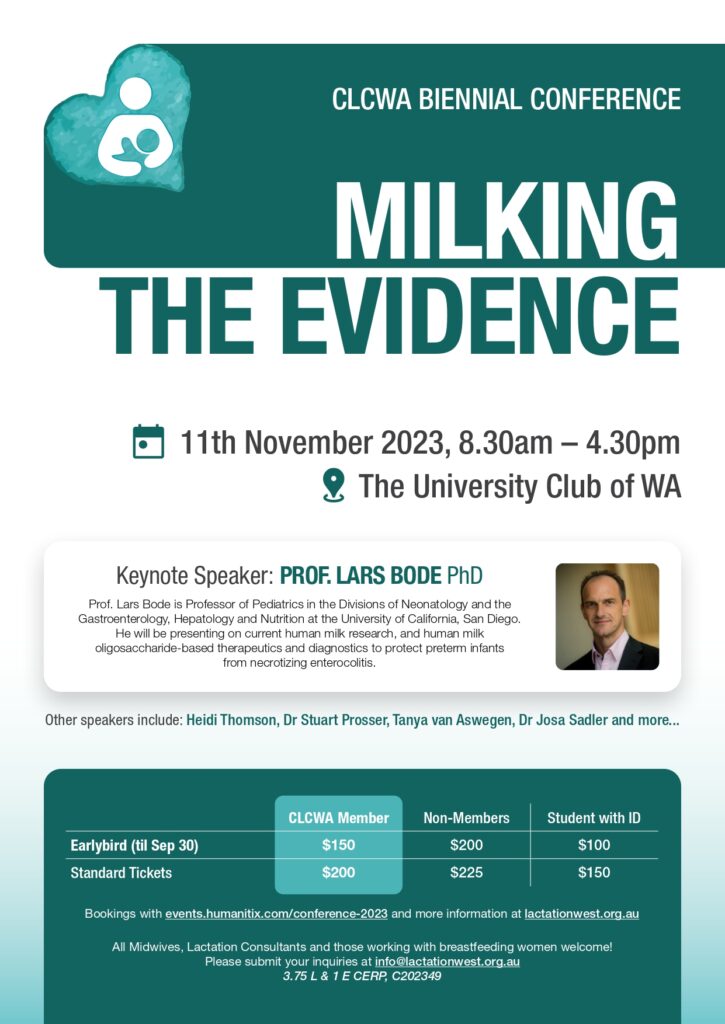
Professor. Lars Bode

Prof. Lars Bode is Professor of Pediatrics in the Division of Neonatology and the Division of Gastroenterology, Hepatology and Nutrition, the Larsson-Rosenquist Chair of Collaborative Human Milk Research, and the founding Director of the Mother-Milk-Infant Center of Research Excellence (MOMI CORE) and the new Human Milk Institute (HMI) at the University of California, San Diego.
Currently, Prof. Bode is leading a research program dedicated to research on breastfeeding and human milk in general and Human Milk Oligosaccharides in particular. Prof. Bode’s main research objectives are to elucidate (i) how milk components are synthesized in the mother’s mammary gland, (ii) how milk composition is affected by external factors such as nutrition, pathogens, or medications, (iii) how milk components affect immediate as well as long-term health and development of infants and mothers, and (iv) how they can serve as natural templates for the development of preventatives, therapeutics, and diagnostics for people of all ages.
Prof. Bode has published over 150 peer-reviewed articles on human milk oligosaccharides and in 2022, he ranked in the top 0.1% of most highly cited scientists in the world.
From Molecules to Systems: A New Area of Human Milk Research
Human milk oligosaccharides (HMOs) are the third most abundant component of human milk discovered almost a century ago. Yet, we are just now starting to understand how these complex sugars are made in the human mammary gland and how they might benefit infant health and development. The presentation outlines our current knowledge on maternal driver and potential infant benefits and paints a picture of the future of human milk oligosaccharide research and application.
Human Milk Oligosaccharide-Based Therapeutics and Diagnostics to Protect Preterm Infants from Necrotizing Enterocolitis
Necrotizing enterocolitis (NEC) remains to be one of the most common and often deadly intestinal diseases in preterm infants. NEC aetiology and pathogenesis are multifactorial and poorly understood, and treatment options are limited. However, we do know that preterm infants who receive human milk are at a six- to ten-fold lower risk to develop NEC, an observation that us to discover a specific human milk oligosaccharide (HMO) called DSLNT that contributes to the benefits of human milk. The presentation outlines our journey from hypothesis to discovery and showcases how the generated knowledge is now driving the development of novel therapeutics as well as point of care diagnostics for optimized human milk nutrition with the ultimate goal to further reduce the number of infants suffering and dying from this devastating disorder.
Dr Chris Mullally
Chris is an early-career researcher at the Centre for Molecular Medicine and the Harry Butler Institute at Murdoch University. He recently completed his PhD at the University of Western Australia where he studied meningococcal disease. His current research focuses on sepsis diagnosis and prevention in both adults and neonates.
Maternal vaccination: A Potential Strategy for Newborn Protection Against Infectious Diseases
Respiratory diseases such as pneumococcal disease, meningococcal disease, and influenza are leading causes of death globally for children less than 12 months of age. While vaccines are available for these diseases, they are ineffective in the early months of life due to the infant’s immature immune system. Maternal vaccination has emerged as a promising strategy to confer protective immunity to infants against various infectious diseases.
Breast milk, a vital source of nutrition for newborns, plays a pivotal role in the transmission of maternal antibodies to the infant. Immunoglobulin A (IgA), immunoglobulin G (IgG), and other immunological components present in breast milk provide essential protection against pathogens. Maternal vaccination stimulates the production of pathogen-specific antibodies, which are subsequently secreted into breast milk, conferring passive immunity to the infant during the critical early months of life. In addition to breast milk-mediated immunity, maternal vaccination induces the production of transplacental antibodies that cross the placenta during pregnancy. The transfer of maternal antibodies provides infants with protection against certain infectious agents before they develop their own active immune responses.
Pneumococcal disease, predominantly caused by Streptococcus pneumoniae, poses a significant threat to infant health. Maternal vaccination against pneumococcal antigens has been shown to elicit protective antibody responses. These specific antibodies are transmitted to infants through both breast milk and transplacental transfer, enhancing their defence against pneumococcal infections.
Influenza, a highly contagious respiratory illness, can have severe consequences for infants, especially those under six months who are ineligible for influenza vaccination. Maternal influenza vaccination, particularly during pregnancy, stimulates the production of influenza-specific antibodies that are effectively transferred to the foetus, safeguarding them during the early vulnerable stages of life.
Meningococcal disease, caused by Neisseria meningitidis, remains a serious public health concern, particularly among young infants. Maternal vaccination against meningococcal serogroups can lead to increased levels of specific antibodies in breast milk and transplacental transfer of protective antibodies. These transferred antibodies have been demonstrated to confer a degree of protection against meningococcal disease in neonates. However more research is needed to demonstrate the efficacy of these vaccines in maternal vaccination programs.
In conclusion, maternal vaccination stands as a promising approach for safeguarding infants against meningococcal disease, pneumococcal disease, and influenza. The transfer of pathogen-specific antibodies via breast milk and transplacental transfer of antibodies plays a crucial role in enhancing the immune defence of infants during the critical periods of vulnerability. Continued research and public health efforts are warranted to optimize vaccination strategies and ensure a robust and sustainable means of protection for infants against these infectious diseases.
Tracey Sedgwick

Tracey is a Registered Midwife, Registered Nurse and International Board Certified Lactation Consultant with extensive experience in neonatal nursing and human milk banking at King Edward Memorial Hospital’s Neonatology Clinical Care Unit. Tracey has worked at the Perron Rotary Express Milk (PREM) bank since it’s inception in 2006 and her current role is Clinical Nurse Specialist / Lactation Consultant. She works closely with neonatologists, a team of NICU lactation consultants, neonatal nurses and milk donors to ensure the safe provision of donor milk as well as lactation care of mothers of preterm infants.
Human Milk Banking in WA
Tracey will share with us the history of human milk banking in Western Australia, the process of donor screening, testing and pasteurization of donor milk, and eligibility criteria for donor milk. Processes for obtaining consent from parents of recipient infants will be explained as well as the lactation care of preterm mothers that have low milk supply and require donor milk supplementation.
Heidi Thomson
RN IBCLC

Heidi is a Registered Nurse and International Board Certified Lactation Consultant with extensive experience working with premature babies and their mothers. After graduating from The University of Notre Dame in 2011 she began her nursing career in Oncology/Haematology, for which she credits the beginning of her determination to provide compassion, empathy and excellence in care. In 2016 Heidi made the move to King Edward Memorial Hospital’s Neonatal Intensive Care Unit. It was here she found her passion for supporting families through the intensive and challenging journey that is prematurity and the NICU environment. Heidi currently works as both a Registered Nurse in the clinical setting and as a Lactation Consultant for the NICU. Prior to her Lactation role, Heidi acted in the position of the Home Visiting Nurse. Whilst in this role she noted a deficit in education to parents regarding their transition home, which ultimately led to implications for their baby. Seeing an opportunity to improve outcomes for the neonates, she prioritised education of both parents and staff in the transitional care of the neonate to the home environment.
Since the birth of her own son Heidi is even more determined to ensure she supports all women and their families with the latest evidence-based practice. She has developed a new appreciation for lactation research, for which she hopes to contribute in the near future.
The Journey Home – Supporting the Preterm Infant and Their Family in the Transition to Exclusive Breastfeeding
The transition from a Neonatal Intensive Care Unit to the home environment can be a daunting and overwhelming challenge for both preterm neonates and their families. For mothers of premature babies who wish to exclusively breastfeed, this transition brings with it a whole other set of challenges. Heidi will discuss the process of preterm infants transitioning to exclusive breastfeeding post their discharge from the NICU, and within this, the special considerations that need to be made and how to best support the mother/baby dyad. She will also give a brief overview of the NICU environment, the importance of educating parents and staff about the transitional period, how to address expectations and normal newborn behaviours, common concerns of both parents and health professionals, and a case study to summarise.
Dr Josa Sadler MD

Josa completed her medical degree at The University of Western Australia and is currently working as a junior doctor with the WA Country Health Service in Albany. She looks forward to one day training as a rural general practitioner with a special interest in women’s and children’s health and moving permanently to Albany to enjoy the fantastic beaches.
Antenatal Attitudes Towards Breastfeeding Differ by Intended Birth Mode
Josa will present on her research project that explored differences in breastfeeding attitudes between Australian women anticipating a vaginal birth, those having a Caesarean birth for medical reasons, and those having a Caesarean birth due to personal preference. Women completed an online survey that included demographic questions, intended birth mode, and the Iowa Infant Feeding Scale. The study findings have implications for breastfeeding education during pregnancy, and support after birth.
Dr Stuart Prosser
MBBS MMed MBA

Dr Stuart Prosser graduated with an MBBS from the University of WA in 2000 before pursuing further studies in Child Health, Women’s Health, Obstetrics and Gynaecology, Anaesthetics and Skin Cancer Management.
Stuart has worked as a Procedural General Practitioner, practising both Anaesthetics and Obstetrics, for over 15 years. During his initial General Practice training he completed his Advanced Diploma in Obstetrics and his JCCA in Anaesthetics. Throughout this period, Stuart has continually focused on enhancing the patient experience.
Stuart holds a Master in Medicine, specializing in perioperative medicine and healthcare systems and leadership, and a Master of Business Administration from the University of Melbourne. He maintains a long-standing commitment to continuous education and serves as an associate professor at Curtin University.
While keenly interested in antenatal care, Stuart also has experience in early pregnancy management (including initial ultrasound) and management of early pregnancy problems (including bleeding and morning sickness). Stuart has a particular interest in the postnatal period and manages all aspects including mental health issues, irritable babies (including sleeping issues), poor weight gain for your baby and any concerns about your recovery after child birth. Stuart also believes partners are a very important, and often ignored, part of the adjustment to parenthood. As such he has a particular interest in partner’s adjustment to parenthood and partner mental health issues.
Stuart is proud to be the Lead General Practitioner Obstetrician (GPO) at Western Obstetrics, a multi-disciplinary practice that provides team-based maternity care. They offer midwifery-led maternity care, with support from GP Obstetricians, and other health services such as women’s health physiotherapists, psychologists, and lactation consultants. Western Obstetrics aims to deliver individualised care that meets the unique needs of each patient. They believe that every patient should receive excellent care during and after the birth of their baby, regardless of whether they deliver privately or publicly.
Women’s Experiences of Breastfeeding after a Caesarean Birth
There is evidence from around the world that Caesarean birth is associated with lower rates of exclusive breastfeeding and shorter breastfeeding duration. However, factors that contribute to these suboptimal outcomes are not well understood. In this presentation, results of a survey of > 1200 Australian women will be presented, including women’s experiences of breastfeeding, post-operative pain and birth satisfaction after a Caesarean birth. Strategies for improving breastfeeding outcomes after a Caesarean birth will be explored.
Tanya van Aswegen APD, MPH

Tanya is a dietitian and public health nutrition specialist with over 15 years of extensive experience in clinical and public health nutrition across diverse cultural landscapes, including the United Arab Emirates, South Africa, and the United Kingdom. She has a BSc Degree in Nutrition and Dietetics and a Master of Public Health degree. Tanya is deeply passionate about protecting, promoting and supporting breastfeeding and has had first-hand experience with the life-saving benefits of breastfeeding and devastating impact of poor infant feeding practices. She has collaborated with the WHO and UNICEF at National and sub-national levels in South-Africa on infant and young child policy development and the implementation of the Baby-Friendly-Hospital-Initiative. She aspires to become a IBCLC in next few years and also pursue research in the field of lactation. Tanya moved to Australia 2 years ago with her family and she is mom to two girls and two dogs.
The Marketing Tactics Shaping a Generation’s Health
The inappropriate marketing of commercial milk formula has shaped our societal and professional norms, values and beliefs around infant and young child feeding. Formula milk marketing, not the product itself, disrupts informed decision making through the deliberate misuse and distortion of scientific information to exploit parental emotions and aspirations. We experience marketing tactics daily, but the marketing of formula milk products is different as choices around infant and child feeding in the first 3 years of life has a profound impact on the lifelong health, development, and rights of both children and their families and should therefore be free of commercial interests and influence. This presentation will look at the latest evidence supporting the importance of The Code of Marketing Breastmilk Substitutes globally, compare The Code to the “Marketing in Australia of Infant Formulas” (MAIF) agreement and discuss the challenges faced in the digital age. It will also explore individual conflict of interest and the role of health care workers in navigating the increasingly pervasive formula milk marketing landscape.
